The consideration of performing a laser surgical procedure on the skin arises when faced with irreversible changes or complex issues requiring comprehensive and combined treatment. Laser dermatosurgery encompasses the capability to address various skin growths, including acne, scars, blemishes, stretch marks, among others.
This method is also effective in performing numerous other dermatological interventions, including oncological procedures.
Laser dermatosurgery is typically carried out using specialized tools and technologies that enable dermatologists to precisely assess the extent of damage and the location of the pathology. Microscopic minimally invasive techniques empower surgeons to operate with minimal disruption to surrounding tissues.
Specifically, we utilize:
Benign skin neoplasms (papilloma, soft fibroma, wart, nevus, birthmarks, keratoma)
Skin scars (post-surgical, post-injury)
Stretch marks
Vascular formations of the skin (hemangiomas, telangiectasias)
Acne and post-acne scars
Pigmentation disorders
Signs of aging on the skin (wrinkles, pigment spots, and more)
Additionally, if needed, our doctors offer consultations not only within Ukraine but also globally, both at our clinic in Kyiv and online by prior appointment. Comprehensive diagnostics, treatment, and preventive measures are provided


Years of experience
Patients
A modern clinic in the center
Successful operations
Unique surgical techniques
Branch of surgery
Units of the latest equipment
Charitable surgical assistance

If you’re experiencing the following symptoms, you should consider consulting a surgeon for laser skin resurfacing (surgery):

The consultation with a surgeon encompasses:
Questioning about symptoms and medical history.
Comprehensive external clinical assessment, including thorough examination, palpation of changed areas, local lymph nodes, and evaluation of each organ system.
Laboratory examinations, encompassing both general clinical tests and specialized tests, including the study of specific tumor markers—substances that help evaluate the likelihood of tumor development.
Instrumental examination, which aims to assess the overall body condition and identify areas with changes. Techniques such as X-ray (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), may be employed.


Laser skin resurfacing
SMAS-lifting (Superficial Muscular Aponeurotic System)
Removal of pigment spots
Normalization of skin pigmentation
Mole removal
Removal of erythema
Viral wart removal
Removal of keratoma
Papilloma removal
Removal of dermatofibroma
Removal of atheroma
Removal of xanthelasma
Lipoma removal
Laser coagulation of hygromas
Removal of telangiectasia
Hemangioma removal
Neoplasm excision
Scar correction
Stretch mark (stretch mark) correction
If you're taking any medications, inform your doctor and consult with them. It might be necessary to adjust or change the dosage.
Maintain a gentle diet and proper hydration a few days before the surgery. If constipated, use laxatives and enemas, and avoid alcohol. This ensures a more predictable reaction to anesthesia and other medications.
Refrain from eating for 6–12 hours before the surgery. Also, avoid drinking, chewing gum, and smoking for 2–4 hours before to prevent stomach contents from entering the respiratory system during anesthesia.
On the surgery day, take a shower and use an enema to cleanse the intestines, preventing involuntary bowel movements due to sphincter relaxation during anesthesia.
Just before the operation:
- remove oral and facial removable items (piercing jewelry, prostheses) to prevent accidental entry into the respiratory system or interference with the procedure.
- take off other items (contact lenses, hearing aids, jewelry) to prevent accidental injuries and damage.
- remove cosmetic products (makeup, nail polish, artificial nails) to aid in visual assessment and automated medical equipment registration.
- empty your bladder and possibly the intestines to prevent involuntary releases during anesthesia.
- change into clinic-provided special clothing.
Additional preparation might occur based on individual characteristics and specific surgical needs.
The main stages:

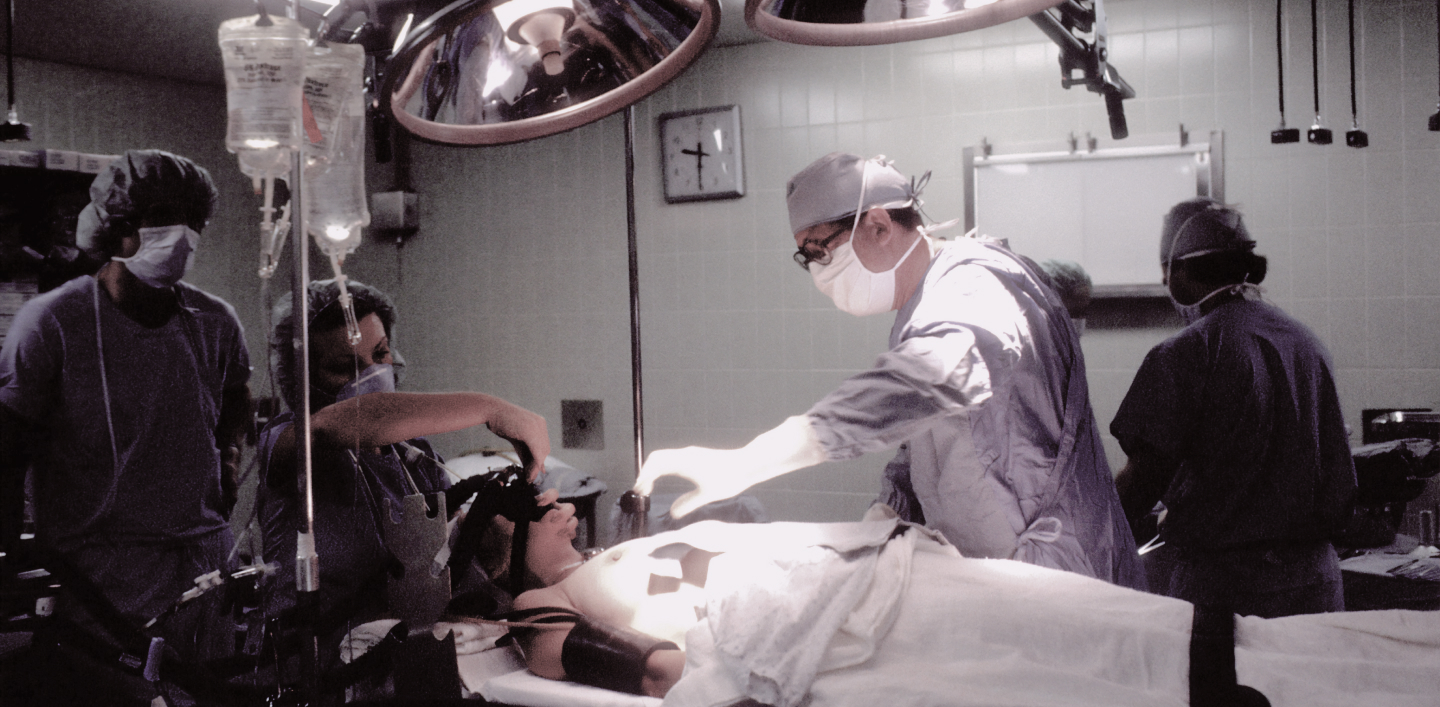
on a gurney or accompanies the staff on foot. In the airlock room, the patient is provided with a medical cap and shoe covers to prevent the entry of microorganisms into the operating room's environment.
a specific composition of the surgical team, carefully tailored to the particulars of each operation.
the patient is positioned on the operating table. Depending on the nature of the operation, the body's position may vary, and the patient is securely fastened using specialized straps.
a vein puncture on the patient's hand, inserting a catheter to administer essential medications. Electrodes are affixed to the patient's body to monitor cardiac electrical activity, while a tonometer cuff is placed on the patient's shoulder to measure blood pressure. Additionally, a sensor is applied to determine the oxygen content in the blood. All of these measures are essential for the continuous monitoring of the patient's condition throughout the anesthesia and surgery.
of the operation are contingent upon the specific objectives, the area of the body undergoing intervention, and align with the chosen surgical approach and technique.

Following the surgical procedure, the patient regains consciousness in the postoperative observation ward. If required, oxygen can be administered through a delicate tube to ensure the body receives an adequate oxygen supply. A nurse will diligently oversee the patient’s condition and, if deemed necessary, administer medications in accordance with the doctor’s instructions.
Prior to the patient’s discharge, the doctor will assess the areas where the intervention took place, collaborate on the approach for subsequent rehabilitation, and provide additional guidance.


Laser facial resurfacing may cause some discomfort or a burning sensation during the procedure, but the level of pain usually depends on several factors, such as the type of laser, procedure intensity, individual skin sensitivity, and pain tolerance.
Various pain relief methods are employed to minimize discomfort during laser facial resurfacing. This can include local anesthesia, skin cooling, or application of soothing creams before the procedure. Some patients might experience minor discomfort during the procedure.
Laser resurfacing is a medical procedure, and patients should discuss all aspects of the procedure with their doctor or plastic surgeon before undergoing it. The doctor will offer recommendations for pain relief and post-procedure care to ensure patient comfort and optimal results.
Laser dermatosurgery can address a range of dermatological issues and cosmetic concerns, including:
For any of these symptoms or conditions, consulting a qualified dermatologist or plastic surgeon is recommended to explore laser dermatosurgery options and receive appropriate advice.
Typically, laser dermatosurgery for scar removal necessitates multiple sessions spaced over weeks or months. The exact duration of recovery and achievement of desired outcomes will be determined by the doctor during the consultation and procedure planning. Variables include scar type, size, individual tissue characteristics, and metabolism.
After laser facial resurfacing, it’s advisable to avoid cosmetics on the first day (to allow the skin to recover). Subsequently, the doctor can provide guidance on when cosmetics can be resumed. Generally, it takes 3-5 days for the skin to heal.
Following laser resurfacing, opt for non-greasy, hypoallergenic cosmetics with a light texture. Avoid products with harsh ingredients, intense colors, fragrances, or active chemicals that could irritate sensitive post-procedure skin.
For concealing redness or imperfections, choose safe skin-toning products like mineral powders or hypoallergenic concealers.
Sun protection is paramount; use high SPF sunscreen and avoid direct sunlight to shield treated skin.
The warranty for laser dermatosurgery covers drugs, medical consumables, and equipment operation. Surgical treatment services are guaranteed in line with medical advancements, clinic specialists’ qualifications, and technical equipment. Final clinical outcomes depend on multiple factors, including individual body characteristics, lifestyle, environment, and stress factors.
Preparation involves consulting a dermatologist or plastic surgeon, discussing expectations, risks, and benefits. The doctor selects the optimal method based on the problem’s nature and skin type, possibly requiring special skin preparation.
Possible complications include temporary pigmentation changes, inflammation, infection, skin dehydration, accidental damage, and allergic reactions to medications. Discuss risks openly with your doctor and follow pre-procedure instructions to minimize potential problems.
A well-prepared operation, highly qualified staff, modern equipment, and coordinated medical team efforts minimize complications’ risks.