The issue of performing facial surgery (surgical treatment of facial injuries) arises in cases of trauma, cracks, fractures, as well as complex problems, etc.
Surgery of maxillofacial trauma is usually performed using specialized tools and technologies, such as computed tomography, magnetic resonance imaging, and other diagnostic methods. This allows the surgeon to accurately determine the extent of the damage and the location of the pathology. Microscopic and endoscopic surgery allow surgeons to perform surgical interventions with minimal damage to surrounding tissues.
Timely and correctly performed treatment of maxillofacial trauma allows patients to return to normal life and maintain or restore its quality.
If needed, our doctors provide consultations not only in Ukraine but also worldwide, both at our clinic in Kyiv and online through prior appointments. Comprehensive diagnostics, treatment, and prevention are offered.


Years of experience
Patients
A modern clinic in the center
Successful operations
Unique surgical techniques
Branch of surgery
Units of the latest equipment
Charitable surgical assistance

You should promptly consult regarding maxillofacial surgery if you experience the following symptoms:

An consultation concerning maxillofacial surgery includes:
interview (the doctor asks about complaints, learns about medical history and life);
external clinical assessment (the patient will be thoroughly examined, palpated, all altered areas and the condition of each organ system will be examined)
laboratory examination (both general clinical tests and special tests);
instrumental examination (to determine both the general condition of the body and those areas where changes have developed);


in case of taking any medications, inform the doctor and agree with him/her (it may be necessary to limit them or change the dosage, regimen)
for several days before the operation, follow a sparing diet, water and drinking regimen; if you have constipation, take laxatives, use enemas and do not drink alcoholic beverages - so that the body reacts more adequately and predictably to anesthesia and other drugs
refrain from eating for 6-12 hours before the surgery, and 2-4 hours before the surgery do not drink, chew gum, smoke - to protect against the ingestion of stomach contents into the respiratory system during anesthesia
on the day of surgery, take a shower, cleanse the intestines with an enema to prevent spontaneous passage of feces during anesthesia due to sphincter relaxation
immediately before the operation –
- removable objects (piercing jewelry, dentures) are removed from the mouth and face so that they do not accidentally get into the respiratory system or interfere with the surgical intervention during the operation
- remove other items (contact lenses, hearing aids, jewelry.) to prevent accidental injury to the body and to prevent them from getting damaged
- remove cosmetics (makeup, nail polish, false nails) from the body to facilitate visual assessment of the body's condition and automated registration with medical equipment
- empty the bladder and, if necessary, the intestines to prevent spontaneous bowel movements during anesthesia
change into special clothes provided by the clinic.
other preparatory measures can be taken in addition, taking into account individual characteristics of the body and the specifics of the surgical intervention
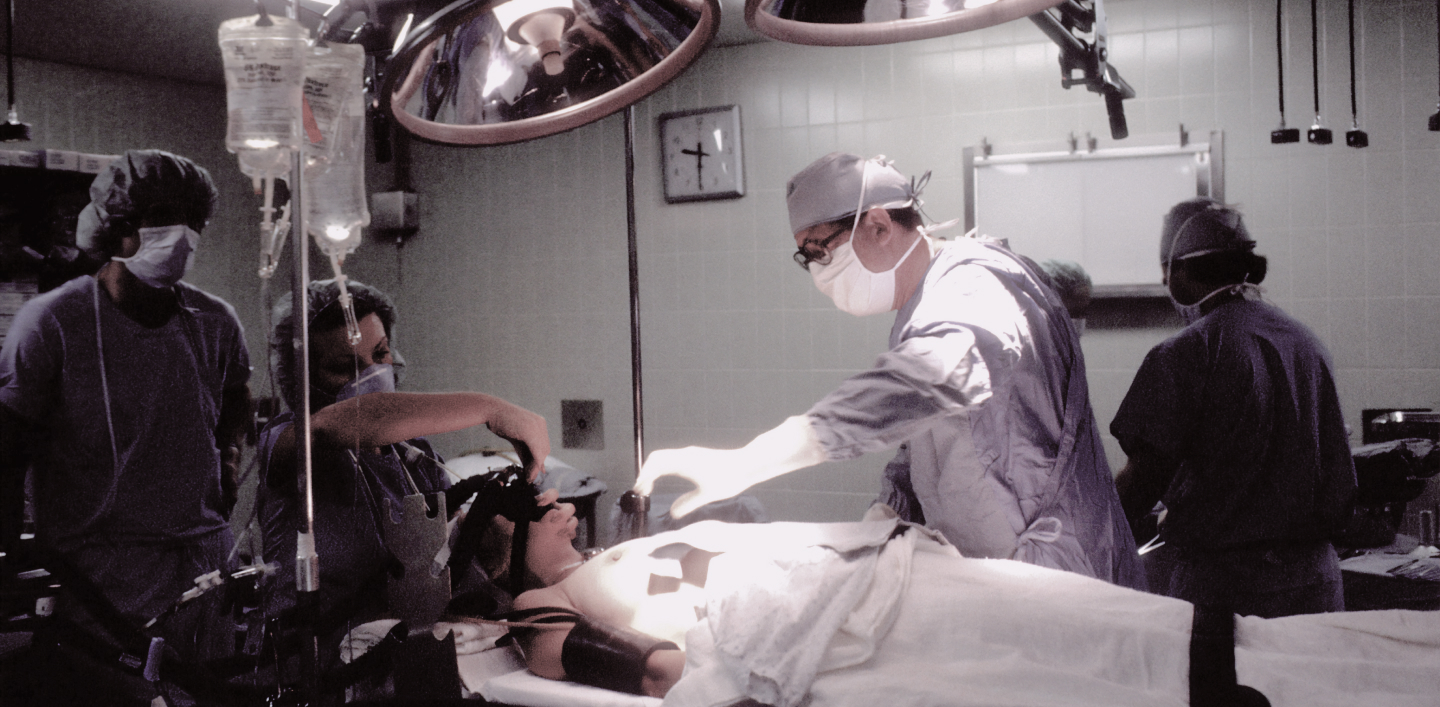
The main stages:

or escorted on foot. At the gateway, they put on a medical cap and shoe covers (to protect against microorganisms in the air of the operating room).
of a certain composition, taking into account the specifics of each operation.
(depending on the specifics of the operation, the body position may differ), and fixed to it with special straps to prevent accidental involuntary movements that would interfere with the operation, as well as to prevent accidental falling of the body from the table.
punctures a vein in the arm, installs a catheter to administer the necessary drugs, places electrodes on the body to monitor the electrical activity of the heart, puts a blood pressure cuff on the shoulder and a sensor on the finger to determine the oxygen content in the blood. All this is necessary for continuous monitoring of the body's condition during anesthesia and surgery.
the area of the body where the intervention is performed, and the specifics of the chosen surgical tactics, technique, etc.

After the operation, the patient wakes up in the ward for postoperative observation. If necessary, oxygen may be administered through a thin tube to ensure that the body has enough oxygen. The nurse will carefully monitor the patient’s condition and, if necessary, use medications agreed with the doctor.
Before returning home, the doctor will examine the postoperative sutures, agree on the tactics of further rehabilitation, and give additional advice.


An oral and maxillofacial surgeon (or dental surgeon, maxillofacial surgeon) treats pathology of the bones of the facial skeleton: congenital defects, acquired defects (cracks, fractures, other injuries), inflammatory diseases, and neoplasms. The specialist can not only restore the functionality lost due to a pathological condition, but also recreate the appearance.
You should visit an oral and maxillofacial surgeon if you have the following in the face: distinct injuries, persistent pain (constant or during chewing, biting), local edema, bleeding, malocclusion after injuries in the absence of effect from orthodontic treatment. Surgery may be performed.
Maxillofacial surgery, facial bone grafting, repositioning of the facial bones and fixation with metal osteosynthesis is required in the following cases: traumas, especially with displacement, and acquired bone deformities.
The warranty for maxillofacial surgery covers implants and other medical consumables and equipment. It guarantees the provision of surgical treatment services in accordance with modern medical advances, the high level of qualification of the clinic’s specialists and the technical equipment of the clinic. The final clinical effect is influenced by many factors that depend not only on the doctor and the clinic, such as individual characteristics of the body, lifestyle, environmental circumstances, and stress factors.
Preparation for maxillofacial surgery includes a preliminary examination and consultation with a surgeon, a comprehensive examination with photo and video analysis of appearance, anthropometry, consultation with related specialists (if necessary), etc. Immediately before surgery, the principles of preparation do not differ significantly from those generally accepted in surgery.
Possible complications after facial surgery include general surgical complications (bleeding and thrombosis, infectious and inflammatory conditions) and more specific to this particular area (postoperative defects, bone nonunion, epileptic syndrome). Careful preparation for the operation, highly qualified experienced medical staff, modern high-tech equipment and well-coordinated work of the team of doctors and other clinic staff minimize the risks of complications.
Contraindications to maxillofacial surgery are conditions whose severity critically increases the risks of surgical treatment, such as infectious, mental, gastrointestinal diseases.